Birth is birth is birth. Regardless of whether you gave birth to your child spontaneously and without any aids, through a gastrointestinal birth or with many interventions and a vacuum extractor, the days and weeks that follow are very individual and difficult to predict. This has less to do with the mode of birth than with the many other circumstances: your mental state, your baby's mood, how much support you have and how the transition to (multiple) motherhood feels for you.
And what we want to tell you here too: All forms of birth are births. And they can be experienced as beautiful and terrible, self-determined and passive, powerful and exhausting. It is OK to want an epidural. It is OK to have a planned cesarean section. It is OK to give birth to your baby in a breech position without painkillers. It is OK to cry because the birth goes completely differently than planned. It is OK to find the cesarean section horrible. It is OK that after the first cesarean section you decide to have it for your second child as well. It is OK to give birth in the tub. It is OK to give all bathtubs a wide berth. It is OK not to glorify birth. It is OK to feel like a goddess after the birth. It is OK to be afraid of the birth. It is OK not to be afraid. It is OK not to want your partner to be there. It is OK to put together the best birth team for you. It's OK not to be able to do it anymore. It's OK to carry on anyway. It's OK to be stressed and to seek help. It's OK to want to tell everyone about the birth. #everythingisOK
But back to the postpartum period. Because: the postpartum period after a Caesarean section can be different in some respects than the first few days after a spontaneous vaginal birth. And because in Germany a lot of children are born via gastrointestinal birth, we want to use this article to prepare you a little for the postpartum period after such a birth. Because - and this is probably the biggest difference: a gastrointestinal birth is an operation that leaves behind a miracle. And it has to heal. That's why it's always good to plan a little extra time for healing - and often also for processing the experiences. But let's start from the beginning:
In hospital after a C-section birth
After a Caesarean section, you will normally stay in hospital for between three and seven days. Immediately after your child is born, the wound will be closed in the operating room, after which you will usually be placed in the delivery room for a while for monitoring. If everything goes well, you will have your baby with you the whole time, you can feed for the first time (if you want to breastfeed) - and they will observe how your body reacts to the operation. If everything is stable, you will then be transferred to the maternity ward.
Shortly before transfer - or on the ward - the bladder catheter, which is always inserted during the operation, is removed. Bladder catheters are used because you cannot control your bladder during a Caesarean section due to the anesthesia. The feeling of bladder control returns after a few hours, however, and then you can do without a catheter. In addition to the catheter, you usually also have a so-called access on your hand or in the crook of your arm. This can also be used to give you painkillers after the operation, which almost all women need in the first few days after the operation. Interestingly, if you are breastfeeding, care will of course be taken to ensure that you only receive medication that is compatible with breastfeeding.
One risk after a Caesarean section - or actually in any postpartum period where you lie down a lot - is the formation of a thrombosis. To prevent this, mobilization usually begins quite early after a Caesarean section. This means that in the hospital you will often get up for the first time on the day of the Caesarean section - with support, of course - and walk a few steps, for example to the toilet. This is often really painful at first because the stitches on and in your stomach start to move. As well as getting up, it can also help to move your feet and hands (in circles, finger and toe exercises), which further stimulates blood flow. In many cases, blood-thinning medication is given or thrombosis stockings are put on to further reduce the risk.
In the past, you could eat light food after a Caesarean section, but luckily those days are long gone. That's why you can eat normally - and ideally drink a lot so that your bowels get moving and you can have a bowel movement for the first time. You should probably avoid food that causes you digestive problems, but that's probably obvious anyway. Some women also experience severe flatulence and constipation after a Caesarean section. It's best to contact the nursing staff in the hospital as soon as you start to feel any symptoms; they can always help with painkillers, laxatives and other tricks.
The first days at home after a caesarean section
Most women go home three to seven days after the Caesarean section. You can still take painkillers, but it's best to discuss this with the people treating you in the hospital before you're discharged. But your midwife can always help you with this too. You can also discuss in the hospital whether you should continue to take thrombosis prophylaxis (medication, compression stockings) at home.
After every birth, it is helpful to have support during the postpartum period: your partner, friends, family or maternity nurse take care of the household, baby, siblings, shopping and visitors while you simply rest. This support is often essential, especially after a Caesarean section, because the pain from the wound means you cannot move as freely as you would after a natural birth. It is also important to take it easy so that the relatively large wound (usually around 15 cm wide and through all layers of tissue) on your stomach heals well.
Scar and scar care after C-sections
After the birth, the wound will be closed and covered with a sterile, self-adhesive wound dressing/plaster. Once the wound has healed superficially - and this usually only takes a few days - this dressing can be removed. This allows air to reach the wound and it can heal even better.
The wound itself is closed with threads or staples, which are either removed in the hospital or at home by your midwife. Sometimes a thread is used that dissolves itself (reabsorbs), so it doesn't have to be done at all. Many women report that clothing (especially trouser waistbands) that press in the seam area are incredibly uncomfortable in the first few weeks. So here too: as comfortable as possible! And please don't be alarmed: there are often several bruises in different "colors" visible around the scar: dark blue, purple or yellowish-green. These are caused by the operation itself and usually disappear quickly. However, if new bruises appear, swelling forms around the scar or the wound itself feels strange, is red, bleeds, etc.: please let your midwife take a look at it! Side note: There are some women who have had very good experiences with scar taping (kinesio taping). If you are interested in this, talk to your midwife!
And as for care: as long as the scar has not yet healed on the surface and is pain-free, the best thing to do is to keep your hands off it! You can occasionally let air get to the scar, but otherwise you shouldn't fiddle around with it too much. As soon as the wound is closed, you can - if you feel like it - massage the scar with a little oil. This touch will not prevent the scar from remaining visible as a line later, but it can be a great help in getting to know this new place on your body. Don't be surprised: a certain numbness around the scar is normal because nerve pathways are also severed during a cesarean section. This can mean that you don't feel the touch at all at first, just a tickling or tingling sensation. This can continue for up to a few months after the birth and even then it will only slowly get better. And if you have the feeling that nothing is changing, contact your midwife or physiotherapists who specialize in cesarean section scars.
Lochia and recovery after an abdominal birth
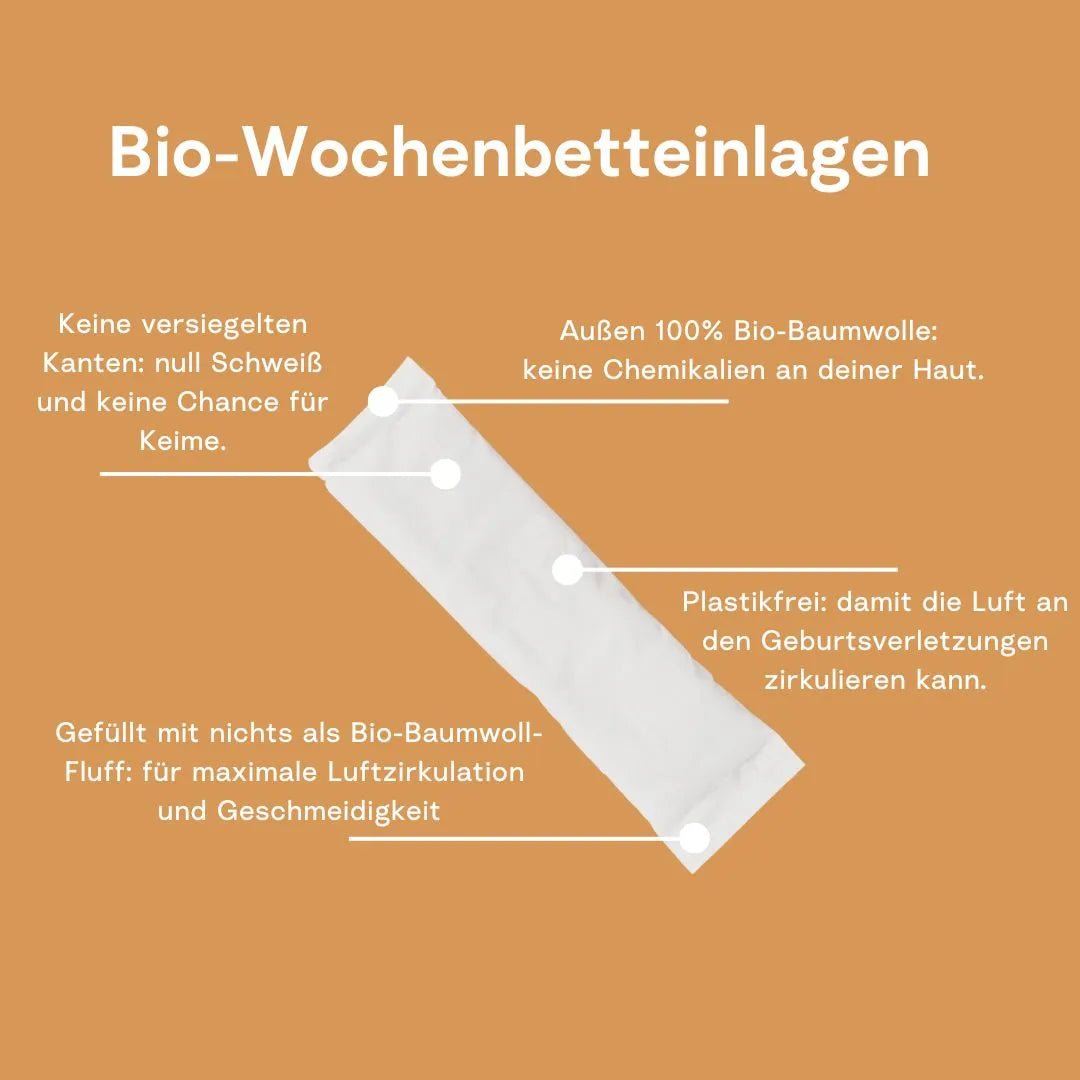
After an abdominal birth, the lochia may be slightly different than after a natural birth - it may be weaker but last a little longer. Weaker because the placenta and mucous membrane are manually removed after the birth of the baby. And longer because the uterus usually takes a little longer to shrink back after a Caesarean section.
On the subject of postnatal recovery: after a Caesarean section, most women start the official postnatal recovery courses paid for by the health insurance companies a little later. It is best to discuss your individual situation with your midwife and then start when it feels good and right for you. Of course, you can also do the first tactile exercises for the pelvic floor beforehand; your midwife can also advise you on this.
If you're now wondering whether you actually need postnatal exercises for your pelvic floor if your child wasn't born through these muscle layers: the pregnancy itself was also a stress test for your pelvic floor muscles and you really deserve a bit of training and a small rebuilding program.