Breastfeeding is awesome. A miracle, so much pain, really practical, sometimes annoying, great nutrition for your child, not for every woman, time-consuming. And above all: breastfeeding is breastfeeding.
Anyone expecting a pro-breastfeeding article will be disappointed. As with almost all issues relating to pregnancy, birth and the postpartum period, we are radically neutral when it comes to breastfeeding: Breastfeeding is great, not breastfeeding is too. Period. Because even though breast milk certainly contains many high-quality ingredients, in our view this only helps if your child and YOU are happy while breastfeeding. Because luckily, if you can't or don't want to breastfeed, there is now also super high-quality pre-food for your baby.
That's why this article contains both: we write about breastfeeding, the difficulties and life hacks surrounding it. And we also give you an overview of alternative ways to feed your child. So that you know your options here too and can decide for yourself what is best for you and your family.
Every woman can breastfeed - right?
No! Breastfeeding is not an instinct, but a socially learned skill. To learn this well, we would actually need more guidance than we have in everyday life today. And even if we could closely observe hundreds of women breastfeeding, there are many situations in which relaxed and pain-free breastfeeding (because that's how it should be) simply doesn't work, despite help, rest, practice and medication. And that's OK. Just as it's OK to be sad that you can't breastfeed. Or relieved that you've stopped breastfeeding because it cost you so much strength, pain and energy. Breastfeeding is really a challenge and doesn't always work - and that has nothing to do with you not trying hard enough. I promise!
And if I want to breastfeed - how can I learn?
If we could answer that in a few simple sentences, we would probably be very rich. Unfortunately, breastfeeding challenges are so diverse that there are no general answers. But we have written down a few topics for you here that you can work on yourself and discuss with your midwife/lactation consultant:
- In position, baby! Breastfeeding is not only possible while sitting with the baby in your arms (the so-called cradle hold). For some women, this is actually a rather uncomfortable position and can make it difficult to latch on properly at the beginning - especially with large breasts. However, many women do not know that there are many other breastfeeding positions and are often not shown to them in the clinic. The most common positions include: side position (you and your baby lie on your side, facing each other, and you breastfeed with the breast that is "down"), in the football position (your baby lies to your side on a nursing pillow, under your arm and its legs pointing towards your back. You guide your baby's head with your hand) and back position (you lie on your back or comfortably slightly raised in the curve of the nursing pillow, your baby lies across you with its face on your chest). For more breastfeeding positions, you can of course just try out what works best for you. Or you can talk to your midwife/lactation consultant!
- Sucking and latching technique. Especially if you have sore, painful or severely deformed (flattened, pointed, etc.) nipples during or after breastfeeding, it can be a good idea to have a midwife or lactation consultant look at your latching technique, sucking and the baby's mouth anatomy (tongue tie, etc.). If the pain is intolerable for you, you can help in various ways: take painkillers (please discuss this), use nipple shields or pump in between and replace meals with pumped milk (or pre-milk) with finger feeding or bottle feeding to give your breasts a break. Lip balms with lanolin (for care) or silver shields can also help heal the nipples.
- The amount of milk is not enough. Midwives can tell that the amount of milk may not be enough if your child is not gaining weight or is only gaining weight very slowly. This must also be looked at individually, but there are many ways to supplement the feeding: either between feedings using finger feeding or a bottle and/or during breastfeeding using a so-called breast feeding system: this is a very fine tube that ends up in the baby's mouth together with your breast and feeds small amounts of pumped breast milk or pre-milk into it in addition to the milk from your breast. Midwives and breastfeeding consultants can also advise you here.
- Pain in the breast, fever: please ask your midwife or gynecologist to rule out or treat a blocked milk duct or mastitis! If you have a blocked milk duct, it can help to apply heat before breastfeeding to make the tissue and milk ducts wide and soft. After breastfeeding, a cool compress can be pleasant. Gently expressing the milk and the blocked milk duct can also help. If you experience severe tension in your breasts in the first few days after birth, it could be due to your milk coming in. Some women find that warm or cold compresses - and time - help. The pain and feelings of tension are caused, among other things, by your tissue first getting used to the new milk in your breast and having to stretch a little accordingly.
And what about the bottles?
If you decided during pregnancy that you do not want to breastfeed and that your child should receive breast milk or formula from a bottle, you can tell them when you register at the clinic or birthing center. Depending on the method, you will then be given a tablet after the birth to make weaning easier - or you will be provided with a breast pump. And regardless of whether breast milk or formula is in the bottle, here are a few tips to keep in mind when feeding: your baby should be upright and close to the body of the person feeding it. With the tip of the bottle, you can lightly touch the baby's lower lip and offer him or her the milk - in the best case, the baby will then suck in the bottle teat on its own. This usually works best if the baby has already shown signs of hunger (open mouth, searching movements, rowing with arms and legs, head movements). If you are feeding formula, you will find the exact information on the mixing ratio of water and milk powder on the packaging of the respective manufacturer. And how much does a newborn drink? This varies - but when drinking formula milk, just like with breast milk from the breast or bottle, your child can usually drink it as needed - that is, whenever he or she is hungry.
Last question: what is the WHO recommendation on breastfeeding?
The World Health Organization - and the National Breastfeeding Commission - recommend six months of exclusive breastfeeding for newborns. We don't want to question the fact that breast milk is a top-quality nutrition for your child. And if you and your baby are happy breastfeeding, we are really happy. But we also know that breastfeeding doesn't always work. And because we are very convinced that unhappy breastfeeding mothers really don't have to be, we want to take a little of the pressure off you and say: do it the way that suits you best. Because as the pediatrician and bestselling author Remo Largo writes in "Baby Years": It is irrelevant for the bond between parent and child whether it is breastfed or bottle-fed.
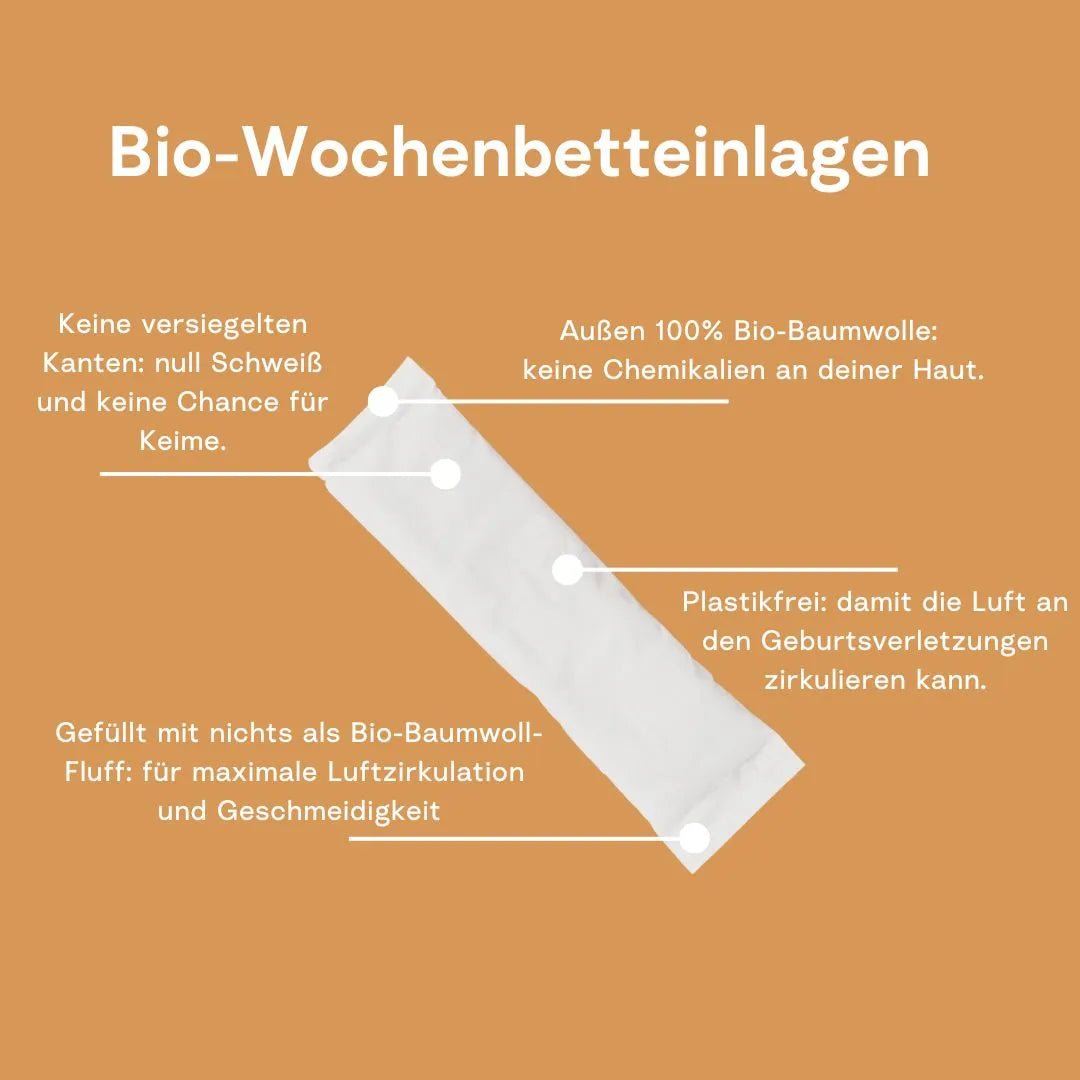
No matter whether and how you breastfeed, pump, wean, supplement or do all of the above at the same time, the weeks are at your side. With our super absorbent nursing pads made of organic cotton and the Nipple Saver, we support you both when breastfeeding and weaning.